How to Diagnose Pancreatitis
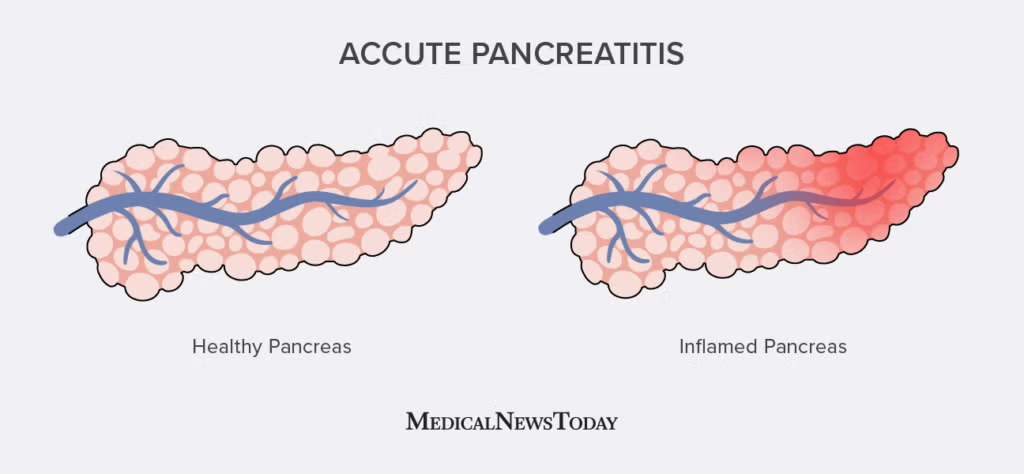
The pancreas is a vital organ. It sits behind your stomach. It makes enzymes. These enzymes help digest food. The pancreas also makes hormones. Insulin is one important hormone it makes. Insulin controls blood sugar. Sometimes, the pancreas becomes inflamed. This condition is called pancreatitis. Pancreatitis can be acute.
How To Diagnose Pancreatitis
This means it comes on suddenly. It can also be chronic. This means it lasts a long time. Pancreatitis can be very serious. It needs prompt medical care. Knowing how to diagnose pancreatitis is essential for doctors. This article explains the steps doctors take. It shows the tests they use. It is important to remember you cannot diagnose yourself. Always see a doctor.
Understanding Pancreatitis
Acute pancreatitis happens fast. Digestive enzymes get stuck in the pancreas. They start to digest the pancreas tissue itself. This causes inflammation. Severe pain results. Gallstones are a common cause. Alcohol abuse is another frequent cause. Other causes exist too. High triglycerides in the blood can cause it. Certain medications can cause it. Infections can cause it. Injury to the abdomen might lead to it.
Chronic pancreatitis develops over many years. It often follows repeated episodes of acute pancreatitis. Heavy alcohol use is a major cause. Genetic disorders can play a role. Blockages in the pancreatic duct can cause it. The pancreas gets damaged over time. It may stop working well. It might not make enough digestive enzymes. It might not make enough insulin. Diagnosing chronic pancreatitis can be different. This article focuses more on acute diagnosis.
Recognizing the Symptoms
Symptoms often prompt a visit to the doctor. The main symptom of acute pancreatitis is severe abdominal pain.
- The pain is usually in the upper abdomen.
- It can sometimes go through to the back.
- The pain often starts suddenly.
- It can get worse after eating.
- Lying flat might make it worse.
- Leaning forward sometimes helps ease the pain.
- The pain can be constant and intense.
Other symptoms commonly happen. Nausea is frequent. Vomiting often occurs too. Fever is possible. A rapid pulse may be present. The abdomen might feel tender or swollen. Some people might look very ill. These symptoms strongly suggest a problem with the pancreas. They are key signals for doctors when considering how to diagnose pancreatitis.
The Physical Examination
When you see a doctor, they will do a physical exam. This exam helps them find clues. They will feel your abdomen. They check for tenderness. They look for swelling or hardness. Pain when the doctor presses the abdomen is a sign. They check your vital signs. This includes your temperature. They check your heart rate.
Blood pressure is measured. A fever or rapid pulse can suggest inflammation. Low blood pressure can mean the condition is severe. Sometimes, if gallstones are the cause, the skin and eyes might look yellow. This is called jaundice. It happens if a gallstone blocks the bile duct too. The physical exam gives the doctor important initial information.
Laboratory Tests (Blood Work is Key)
Blood tests are very important for diagnosing pancreatitis. They look for substances in your blood. Certain enzymes made by the pancreas become high in the blood when the pancreas is inflamed.
- Amylase and Lipase: These are the most important blood tests. Amylase and lipase are digestive enzymes. The pancreas makes them. In pancreatitis, these enzyme levels usually rise significantly in the blood. Levels often become three or more times higher than normal. Elevated lipase levels are often more specific to the pancreas than amylase levels are. High levels of these enzymes strongly indicate pancreatitis.
- Complete Blood Count (CBC): This test checks your white blood cells. An elevated white blood cell count can mean there is inflammation or infection. This is common in pancreatitis.
- Liver Function Tests (LFTs) and Bilirubin: These tests check how well your liver is working. They also measure bilirubin. Bilirubin is a waste product. If gallstones are blocking the bile duct (which is near the pancreatic duct), these levels can be high. This points to gallstones as a possible cause of the pancreatitis.
- Kidney Function Tests: Pancreatitis can affect the kidneys. Doctors check kidney function to see if there are problems.
- Blood Glucose: The pancreas makes insulin. Pancreatitis can affect insulin production. Blood sugar levels might be high.
- Calcium Levels: Calcium levels can sometimes drop in severe cases of pancreatitis. Doctors check this.
Blood tests provide strong evidence. High amylase and lipase are key markers when a doctor considers how to diagnose pancreatitis.
Imaging Tests
Imaging tests create pictures of the inside of your body. They help doctors see the pancreas. They can check for inflammation. They look for causes like gallstones.
- Abdominal Ultrasound: This test uses sound waves. It is good for looking at organs in the abdomen. It is very useful for finding gallstones. Gallstones are a major cause of pancreatitis. Ultrasound can sometimes show the pancreas itself. However, gas in the intestines can block the view of the pancreas.
- Computed Tomography (CT) Scan: A CT scan uses X-rays. It takes many pictures from different angles. A computer puts them together. This creates cross-sectional images. A CT scan is usually the best test for diagnosing acute pancreatitis. It can show if the pancreas is swollen. It can show inflammation. It can detect fluid collections around the pancreas. CT scans also help doctors assess how severe the pancreatitis is. They can find complications.
- Magnetic Resonance Imaging (MRI) / Magnetic Resonance Cholangiopancreatography (MRCP): MRI uses strong magnets and radio waves. It creates detailed images. MRCP is a special type of MRI. It focuses on the bile ducts and the pancreatic duct. MRCP is excellent for finding stones or blockages in these ducts. It uses no radiation. Doctors might use MRCP if they strongly suspect a blockage caused the pancreatitis. It helps decide if a procedure like ERCP is needed.
Imaging gives a visual picture. It confirms what blood tests suggest. It helps doctors see the extent of the problem. This is a crucial step in how to diagnose pancreatitis.
Other Diagnostic Tools
Sometimes, other tests are needed for a full diagnosis or to find the cause.
- Endoscopic Ultrasound (EUS): This procedure uses an endoscope. An endoscope is a thin, flexible tube with a camera. It also has a tiny ultrasound probe on the end. The tube is passed down the throat into the stomach and small intestine. From there, the ultrasound can get very close to the pancreas and ducts. EUS provides very detailed images. It is good for finding small stones or other subtle issues.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): ERCP also uses an endoscope. Dye is injected into the bile duct and pancreatic duct through the endoscope. X-ray pictures are taken. This shows the ducts clearly. ERCP is used to find blockages. It can also be used to treat blockages. For example, doctors can remove gallstones blocking a duct during ERCP. This procedure is more invasive. It is usually done if a blockage is strongly suspected and needs to be cleared. It is both a diagnostic and therapeutic tool for certain causes of pancreatitis.
- Stool Tests: These are not common for acute pancreatitis. But for chronic pancreatitis, doctors might check stool. They look for fat. If the damaged pancreas is not making enough digestive enzymes, fat is not absorbed well. It appears in the stool. This test helps diagnose the digestive failure aspect of chronic disease.
These tests provide more detailed information. They help doctors pinpoint the cause and the exact condition.
Diagnostic Criteria
Doctors typically use a set of criteria to confirm acute pancreatitis. Usually, a diagnosis is made if a patient meets at least two of these three conditions:
- Characteristic abdominal pain (as described earlier).
- Elevated levels of serum amylase or lipase (at least three times the upper limit of normal).
- Findings on imaging (especially a CT scan) that show changes consistent with pancreatitis.
Meeting two out of these three points is generally enough to confirm the diagnosis of acute pancreatitis.
Considering Other Possibilities
Doctors must also think about other conditions. Many other problems cause abdominal pain. This is called the differential diagnosis. Conditions like appendicitis, gallstones without pancreatitis, a stomach ulcer, a heart attack, or problems with the intestines can cause similar pain.
Doctors use the physical exam, blood tests, and imaging results to rule out these other possibilities. The combination of typical symptoms and high pancreatic enzymes is usually very specific to pancreatitis.
Pancreatitis, an inflammation of the pancreas, is a serious medical condition. Knowing how to diagnose pancreatitis involves several steps taken by a qualified healthcare professional. It starts with recognizing the characteristic severe abdominal pain and other symptoms. The physical examination provides initial clues.
Key blood tests, especially measuring amylase and lipase levels, offer strong evidence of pancreatic inflammation. Imaging tests, most commonly a CT scan, allow doctors to visualize the pancreas, confirm inflammation, and assess severity. Other tests like ultrasound, MRI/MRCP, EUS, or ERCP may be used to find the cause or evaluate complications.
Diagnosing pancreatitis relies on combining clinical signs, blood work results, and imaging findings. If you experience sudden, severe abdominal pain or other symptoms suggestive of pancreatitis, you must seek immediate medical attention. Early diagnosis and treatment are crucial for managing pancreatitis effectively and preventing complications.
This information helps you understand the diagnostic process but is not a substitute for professional medical evaluation. Always consult a doctor for any health concerns.